Suffering from heartburn or reflux? Your stomach acid isn’t the problem.
“I would like to find a stew that will give me heartburn immediately, instead of at three o clock in the morning”
John Barrymore
Introduction
Acid reflux (aka ‘heartburn’) and GERD (Gastrointestinal Reflux Disease - a more serious form of acid reflux) is the most common digestive disorder (1). Studies show that 10-20% of individuals experience symptoms at least once a week, and the prevalence of GERD is increasing steadily.
Up until recently heartburn wasn’t taken too seriously. But we now know that heartburn and GERD can have serious and even life-threatening complications, including scarring, constriction, ulceration and ultimately cancer of the esophagus. But as well as creating upward problems for the esophagus, it also creates downward problems in your digestive tract, such as IBS and even stomach cancer. So why not just get rid of stomach acid?
Believe it or not, stomach acid is not there just to punish you for eating spicy food. It is in the stomach because it needs to be there. It is found in the stomach of all vertebrates. And while it isn’t necessary for life, it is certainly a requirement for health.
Most people have no idea just how many vital roles stomach acid plays in our bodies. Such misunderstanding is being perpetuated by drug companies who continue to insist that stomach acid is not essential. Stomach acid IS essential - for preventing bacterial overgrowth, for nutrient absorption, for digesting protein and fat, for absorbing carbs, for preventing infection and for neutralising toxins in what we consume. We nuke it at our peril.
What is heartburn/acid reflux/GERD
This is when stomach acid is forced up through the valve at the base of the esophagus and burns its delicate lining. The condition is characterised by a burning sensation in the chest that has coined the term “heartburn”.
If you ask the average Joe on the street what causes heartburn, he’ll tell you “Too much stomach acid”. Typically, that is the diagnosis of doctors too – based purely on symptoms, without performing a test for stomach acid levels.
But there is a big problem with this theory: the incidence of heartburn and GERD increases with age, while stomach acid levels generally decline with age. In one study, researchers found that over 30% of people over 60 suffer from atrophic gastritis (age-related stomach acid decline, due to loss of the cells that produce stomach acid). Another study found that 40% of women over 80 produced no stomach acid at all. The fact is that when stomach acid is measured in people suffering from heartburn or GERD it is almost always low, not high.
Jonathan Wright MD, author of the book Why Stomach Acid is Good for You, explains:
‘When we carefully test people over age forty who’re having heartburn, indigestion and gas, over 90 percent of the time we find inadequate acid production by the stomach’.
In 25 years of conducting these tests, he found very few people with excess stomach acid, and hardly ever associated with GERD.
In fact, any amount of acid in the esophagus is going to cause problems. That is because its delicate lining isn’t protected against acid like the stomach lining is. Just because you have heartburn, it doesn’t mean you have excess acid, it means some of your acid has got into the wrong place.
What exactly is Stomach Acid for?
Normally, a healthy stomach creates a strongly acidic environment with a pH of between 1.0 and 2.5.
1) We need it for optimal digestion and absorption
Stomach acid is a prerequisite for healthy digestion – the breakdown and absorption of nutrients occurs only within a narrow range of acidity in the stomach. If there isn’t enough acid, whether natural or as a result of using drugs, the normal chemical reactions required to absorb or activate several key nutrients are significantly impaired.
Stomach acid is necessary for the following:
to trigger the production of pepsin, an enzyme required to break down proteins into their component amino acids and peptides - these are needed for manufacturing hormones and neurotransmitters.
to prep Vitamin B12 so it can be absorbed in the small intestines - without which we will experience fatigue, neuropathy and cognitive decline;
for the correct secretion of both pancreatic and gallbladder digestive fluids, essential for the digestion and absorption of carbs, fats and proteins;
to separate out tightly-bound minerals (eg iron, zinc, magnesium, chromium, calcium) from protein, to allow for absorption in the intestines - insufficient mineral uptake can, over time, lead to a myriad disease states from anemia to Type 2 diabetes to arthritis, depression, osteoporosis, hypothyroidism, autoimmune conditions. In one study, 35 of 40 people with chronic iron-deficiency anaemia, were found to have below normal stomach acid secretion.
2) It’s our first line of defence
Although our mouths, throats and intestines are teaming with hundreds of species of bacteria, a healthy stomach is normally almost completely sterile. Why? Because stomach acid kills bacteria. Arguably stomach acid’s most important role is to protect the stomach and digestive tract from pathogenic (harmful) bacteria that are present in the food or drinks we consume or the air we breathe. At the same time stomach acid also prevents good bacteria in the intestines from moving up into the stomach and esophagus where they can cause problems. The low pH (high acid) environment of the stomach is one of the major defence mechanisms of the body. When the pH of the stomach is 3 or lower, (which is the normal, between-meal resting level) bacteria don’t last more than fifteen minutes. But when stomach acid is too low and the pH of the stomach rises above 5, bacteria begin to thrive. The conditions are perfect.
What causes heartburn (or acid reflux or GERD)?
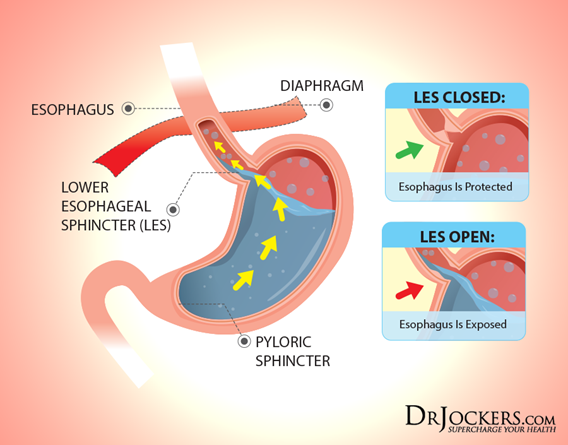
The prevailing scientific theory is that GERD is caused by dysfunction of the muscular valve (sphincter) that separates the lower end of the esophagus and the stomach. This is known as the Lower Esophageal Sphincter or LES. The LES normally opens wide to permit swallowed food and liquids to pass into the stomach. Except for burping, this is the only time that the LES should open. If the LES is working properly, it doesn’t matter how much acid we have in our stomachs, it’s not going to make it back up into the esophagus. But if the LES is not working properly, as in GERD, acid from the stomach gets pushed up into the esophagus and damages its delicate lining - and it hurts.
Acid reflux is not evidence of excessive stomach acid; its evidence of stomach acid in the wrong place!
So what is causing the LES to malfunction?
Over time that valve can become weaker, due to one (or more) of a number of things: i) overeating or being overweight, either of which puts a lot of extra pressure on the LES, ii) smoking which damages the membranes in the LES causing it to weaken, iii) alcohol, regular consumption of which relaxes the muscles in the LES reducing its ability to close, iv) certain medications which cause the LES to relax, including PPIs and inhalers used to treat asthma.
But a weakened LES doesn’t, in and of itself, cause acid reflux. Acid reflux occurs when gas, originating in your intestines, causes stomach bloating that pushes the stomach contents, including acid, up through the weakened LES into the esophagus (1).
So what causes the bloating?
Bloating is caused by maldigestion or gut dysbsiosis (imbalance of gut microbes or microbes in the wrong place). There are a number of causes of these conditions, with the principal one being, ironically, low stomach acid!
Low stomach acid causes bacterial overgrowth
As we showed earlier, one of the main roles of stomach acid is to inhibit bacterial overgrowth. At a pH of 3 or less (the normal pH of the stomach) most bacteria can’t survive more than 15 mins. But when stomach acid is too low and the pH of the stomach rises above 5, bacteria begin to thrive. This will also disrupt the delicate balance and function of the small intestine, causing SIBO (small intestinal bacterial overgrowth).
Low stomach acid causes malabsorption of carbohydrates
We have already talked about the fact that stomach acid supports the release of pancreatic enzymes into the small intestine where much of what you consume is absorbed. If the pH of the stomach is too high (due to insufficient stomach acid) those enzymes will not be secreted and macronutrients will not properly broken down and therefore malabsorbed.
Well, if carbs are not absorbed in the small intestine, they will be fermented by the microbes in your large intestine (or even in the small intestine if you suffer from SIBO). This fermentation produces gas which causes bloating, which is the driving force behind acid reflux and GERD. From Dr Norm Robillard’s brilliant book Heartburn Cured just 30g of carbohydrate that escapes absorption in a day can produce more than 10,000 ml (10 litres) of hydrogen gas. That is a huge amount of gas!
But when stomach acid is sufficient, and carbs are consumed in moderation, they will be properly broken down into glucose and rapidly absorbed in the small intestine before they can be fermented by microbes. Increasing stomach acid and limiting carb intake have both been shown to greatly improve, and in some cases completely cure, acid reflux and GERD.
Bacterial Overgrowth + Malabsorbed Carbs = GAS!
Finally, then, what causes low stomach acid (technically called ‘hypochlorhydria’) ?
Partly age - stomach acid production naturally declines with age.
H Pylori bacterial infection (this is intentionally listed first under Connections at the end of this article)
Protein Pump Inhibitors (eg Omeprazole) and other acid suppressing medications
Chronic stress directly causes a reduction in stomach acid secrretion
Poor eating hygiene (this means eating when you are rushed, eating when you are stressed, and poor chewing)
Nutrient deficiencies, in particular zinc, magnesium and B vitamins
Regularly consumed allergens promotes gut inflammation that in turn results in suppressed stomach acid
What is the mainstream medical approach to heartburn and GERD?
The mainstream medical approach involves taking acid-suppressing drugs. These are protein pump inhibitors, or PPIs, which permanently block an enzyme that tells your stomach to produce acid. These drugs are typically prescribed for as long as symptoms are present.
However, as I hope you all now know, symptom relief doesn’t mean that the underlying cause of the problem is being addressed. Too often western medicine focuses on suppressing symptoms without paying attention to what is causing the symptom to appear in the first place. The misguidedness of this approach is outstandingly demonstrated in the case of heartburn and GERD, where acid-inhibiting drugs are used to treat conditions that are cause by insufficient stomach acid!!
This conventional treatment not only fails to address the underlying cause of heartburn/GERD but actually nearly always makes it worse. One study using young people who didn’t suffer from reflux, gave them PPIs for 3 months, and when they came off them, they all got reflux! In other words, they create the problem that they are designed to treat. This means that people who start taking acid-suppressing meds often end up taking them for the rest of their lives.
The negative effect of these drugs I have set out below. These must have been known to the pharmaceutical companies, for when PPIs were first introduced, it was recommended that they were not taken for more than 6 weeks. This prudent advice would appear to have been discarded, as it isn’t uncommon today to find people who have been on these drugs for decades, not weeks.
Drugs for acid-reflux are cash cows for pharmaceutical companies. PPIs generated more than $12bn a year in 2018 in the US alone, and according to Bloomberg, this was expected to grow by $3.2m between 2019 and 2023 (2). I expect the UK figures are not dissimilar on a pro-rated basis. The last thing they want is for doctors and their patients to learn how to treat heartburn and GERD without them! And since 2/3 of all medical research is sponsored by drug companies, its virtually guaranteed that we won’t see any large studies on the effects of a low-carb diet on acid reflux.
However, the good news is that you are reading this article and you will now understand that both heartburn and GERD are easily prevented and cured by making simple dietary and lifestyle changes.
So how, exactly, do acid-suppressing drugs cause problems?
Because they work. They do just that. They suppress our precious stomach acid!!
Remember that its our first line of defence? And when the pH of the stomach is 3 or lower bacteria don’t last more than fifteen minutes? Well, as the pH rises to 5 or more, many bacterial species can avoid the acid treatment and begin to thrive. This is precisely what happens when you take PPIs or other acid-suppressing medication. This leads to bacterial overgrowth in the gut, and although this won’t kill you (at least not right away) it will make you far more vulnerable to serious bacterial infections and weaken your immune system’s ability to fight off such infections once you have them. Researchers in Italy detected SIBO (small intestinal bacterial overgrowth) in 50% of patients using PPIs compared to 6% of healthy control subjects (3).
Remember its essential for digestion of protein digestion? When stomach pH becomes less acidic (ie more alkaline) it screws up the action of pepsin, and as a result proteins don’t get broken down. This allows large protein molecules to get into the small intestine and creates major strain on the pancreas to produce enough enzymes to metabolise them. This ultimately wears out the pancreatic enzyme stores and creates stress and irritation throughout the gut. At the same time, proteins that escape digestion by pepsin may end up in the bloodstream as a result of Intestinal Permeability (aka Leaky Gut). Since this isn’t supposed to happen, the body reacts to these proteins as if they were foreign invaders, causing an immune response and systemic inflammation, ultimately giving rise to autoimmune disease.
Remember its essential for nutrient absorption? Here is a good example of acid-suppressing drugs getting in the way of this: B12 is needed for normal nerve activity and brain function; a number of studies have examined the negative effect of PPI therapy on B12 absorption - in one study on healthy subjects treated with 20 mg and 40mg of a PPI for two weeks, B12 absorption was reduced by 72% and 88% respectively.
Can’t I just make my heartburn go away with Gaviscon?
Many people use antacids to relieve the pain of heartburn. This may give you temporary relief from the symptoms, but then more acid is automatically produced to bring the stomach back to its intended pH. It therefore does nothing to fix the actual problem. In the meantime the low acid environment (high pH) that you have created in your stomach is causing all the problems listed above.
If you need some rapid relief, for a short period of time, or if you suffer from acid reflux on an occasional basis, dissolve 1/4 tsp of baking soda in 1/2 cup of water, or drink a cup of slippery elm tea.
Three steps (without drugs) for curing Heartburn and GERD forever!
Curing a disease means eliminating its cause. When a disease is cured, the symptoms don’t return once the treatment is removed.
To sum up, heartburn/acid reflux/GERD is not caused by too much stomach acid. It is caused by too little stomach acid and bacterial overgrowth in the stomach and intestines. Therefore successful treatment is based on restoring adequate stomach acid production and eliminating bacterial overgrowth.
1) Adopt a low carb diet.
A high carb diet promotes bacterial overgrowth, which in turn suppresses stomach acid (in particular if you have H. pylori infection). This creates a vicious cycle where bacterial overgrowth and low stomach acid reinforce each other in a continuous decline of digestive function (4). The longer chain carbs (disaccharides and polysaccharides) are the ones that feed the bad bacteria in our gut, whereas the short chain carbs (monosaccharides) don’t cause a problem. In practice that means you should eliminate all grains, legumes and starchy vegetables, but fruits and non-starchy root vegetables such as squash, swede, turnips, beetroot, carrots, can all be eaten.
Be careful to avoid processed low-carb foods sold in supermarkets. Processed foods tend to contain many additives, preservatives, emulsifiers, gums and other artificial ingredients that will make your digestive symptoms even worse. Eat whole foods selected from the outside aisles of the supermarket.
Fructose and artificial sweeteners have been shown to increase bacterial overgrowth. Artificial sweeteners should be eliminated completely, and fructose should be reduced to what occurs naturally in fruit.
High fibre diets are healthy for everyone except those suffering from bacterial overgrowth. Virtually none of the fibre we consume is absorbed, but rather passes through to the colon and instead becomes food for your intestinal bacteria. This is great if you have a healthy gut microbiome, but if you have bacterial overgrowth, (or ‘dysbiosis’) this only fuels the enemy. For the same reason you should avoid prebiotics, which is simply food for your microbes in a pill format – great if you haven’t got bacterial overgrowth, but otherwise it will increase the amount of gas you produce in your gut.
While I am at it, you should cease to eat the foods that cause your LES to spasm. The most commone triggers are cooked tomato sauce, citrus juices, coffee, black tea, alcohol, spicy foods, fried food, chocolate, and things with mint in (toothpaste, tea or gum). Eliminating these while working on the other root causes can bring welcome rapid relief.
2) Replace your stomach acid and take digestive enzymes
There is a reasonably reliable “low-tech” method that can be performed at home to determine whether hydrochloric acid (HCL) supplementation will provide a benefit. To do this, get some HCL capsules that contain pepsin (it’s always a good idea to take HCL with pepsin). Start with one 500mg capsule of HCL w/ pepsin, taking it after the first few mouthfuls of each meal. If you don’t feel a mild burning sensation, on day 2 increase the dose to two capsules, then the next day to 3 capsules. Carry on increasing the dose gradually by one capsule (up to a max of 8 capsules) until you feel a mild burning sensation in your chest. At this point reduce the dose to the previous dose and stay at that dosage. Overtime you may find you can reduce the dose further.
Jonathan Wright MD, (referenced above), and many other clinicians have found that giving HCL supplements to patients with heartburn and GERD nearly always cures their problem.
‘In 24 years of nutritionally oriented practice, I’ve worked with thousands of individuals
who’ve found the cause of their heartburn and indigestion to be low stomach acidity. In
nearly all these folks, symptoms have been relieved and digestion improved when they’ve
taken supplemental hydrochloric acid and pepsin capsules’. Why Stomach Acid is Good for You
[Note: HCL should never be taken by anyone who is also using any kind of anti-inflammatory medication such as corticosteroids, or regular doses of paracetamol, ibruprofen or other NSAIDs. These drugs can damage the gastrointestinal lining and supplementary HCL will aggravate that, increasing the risk of gastric bleeding or ulcer.]
I also recommend taking broad spectrum mix of digestive enzymes. Such a supplement will support the digestion of protein, carbohydrates, fat, fibre and lactose.
Another way to stimulate acid production in the stomach is by taking bitter herbs. “Bitters” have been used in traditional cultures for thousands of years to stimulate and improve digestion. More recently studies have confirmed the ability of bitters to increase the flow of digestive juices, including HCL, bile, pepsin, gastrin and pancreatic enzymes. Bitters are normally taken in very small doses – just enough to cause a strong taste of bitterness.
Apple cider vinegar (or lemon juice) is also effective. Sip1 tbsp in 4 oz of water throughout a meal. ACV has natural acetic acid that helps to reduce the pH of the stomach and it also activates the vagus nerve, which turns on the production of stomach acid, bile and pancreatic enzymes.
It is important to avoid consuming more than a small glass of liquid during meals. Water is especially problematic, because it literally dilutes the concentration of stomach acid. Drink water up to 15 mins before a meal and then ideally wait until 2 hours afterwards. Wine, on the other hand, in moderation, is fine and may even be helpful.
Lastly slow down, sit down, and chew chew chew. This is what we call ‘eating hygiene’. On average we chew each bit of food only a few times before swallowing it down, often with several gulps of water as a chaser. Many of us eat so quickly that meals feel like a race - an annoying must-do to put hunger at bay. However, a meal time can be a very real form of self-care and health-care. Try to chew your food until it’s mostly liquid. This significantly reduces the work of your stomach. You would be amazed at the great results of people with acid reflux who just change these two things - chewing their food 20-30 times per bite and not drinking too much liquid with meals.
3) Restore beneficial bacteria and a healthy mucosal lining in your gut
Because bacterial overgrowth is such a major factor in heartburn/GERD, restoring a healthy balance of intestinal bacteria is an important part of treatment. Beneficial bacteria (probiotics) are key to protecting against potential pathogens, by redressing the balance (ie outnumbering them). Probiotics have been shown to be effective in reducing bacterial overgrowth and in treating Crohn’s disease, ulcerative colitis and other digestive disorders (5). They have also been shown to significantly increase the cure rate of treatment for H. Pylori (6) (see ‘Connections’ below).
Even better would be to eat fermented foods daily. Fermented foods have been consumed for their probiotic effects for thousands of years. Contrary to popular belief, foods like yoghurt and kefir have a much higher concentration of beneficial microbes than probiotic supplements do. Its best to make them at home as the microbe count will be much higher. If dairy doesn’t work for you, raw sauerkraut or kombucha are good alternatives, both of which can be made easily at home.
If you do need to use commercial probiotics, go for a spore-based, broad spectrum probiotic, if you can. This one has a 5 yr shelf life and doesn’t require refrigeration, plus maintains its efficacy during antibiotic treatment. Just be careful if you have SIBO not to use a product which contains Lactobacillus acidophilus, as these can make the condition worse.
In order to restore your healthy gut lining, which is another important part of recovering from heartburn/GERD, you need to do your best to avoid chronic stress and medications such as steroids, calcium channel blockers, benzodiazepines and NSAIDs (non-steroidal anti-inflammatory drugs, ie ibruprofen and paracetamol). All of these suppress prostaglandin production, important for modulating stomach acid, so it is vital for anyone dealing with any type of digestive problem (including GERD) to find ways to manage their stress and avoid the use of NSAIDs as much as possible.
Homemade bone broth is brilliant at restoring a healthy mucosal lining in the stomach, as is Deglycyrrhised Liquorice (DGL) - which unsurprisingly appears to be effective in treating gastric and duodenal ulcers, working as well as H2 blockers but with far fewer side effects and no undesirable acid suppression. It has even been shown in animal studies to protect the stomach lining from damage done by NSAIDs (7). Lastly Slippery Elm and Marshmallow are good for soothing the gut lining.
Coming off PPIs
If you are coming off acid-suppressing drugs after several years, you need to do it very very slowly - if you are taking them 7 days a week, only remove one day at a time. After two weeks remove another day, and supplement with a little bit of antacid if you need to. Chewable liquorice is good; it protects the gut from the excessive stomach acid that may occur as you reduce the drugs. Also marshmallow root: take 2–5 mL of liquid marshmallow extract 3 times per day to help build up the mucus lining of the stomach that will protect the stomach lining from being hurt by the new influx of stomach acid.
It may be necessary to replace the nutrients that are not absorbed without sufficient stomach acid. These include B12, folate, calcium, iron and zinc. It is best to get your levels tested by a qualified nutritionist or functional practitioner, who can then help you replace them through diet and/or supplementation.
Last resort
There may be some cases when an entirely natural approach is not enough. When there is tissue damage in the esophagus, for example, a surgical procedure called “gastroplication” which repairs the LES valve may be necessary. This procedure doesn’t have the potential to create nutrient deficiencies and disease the way that acid blockers do.
Connections
If you have got this far and are still interested, you might wish to skim down this list of conditions that are connected to heartburn or GERD. I would encourage you to at least read the first one:
Connection between GERD and H. Pylori
H. Pylori is short for Helicobacter Pylori and is a sophisticated microorganism that can infect your stomach. It has incredible adaptive advantages that gives it the ability to survive in the stomach’s harsh environment. It can damage the tissue in your stomach and the small intestine, causing inflammation throughout the gut (gastritis), gastrointestinal permeability (‘Leaky Gut’) and in a few cases peptic ulcers in the small intestine. It plays a significant role in GERD and other digestive disorders. Untreated it can contribute to stomach cancer (see below).
We know that H. pylori suppresses stomach acid secretion. In fact, this is how it survives in a hostile acidic environment like the stomach, which would ordinarily kill all bacteria. But particularly relevant to those who are taking acid-suppressing drugs, researchers have shown that the initial infection with H. pylori can only take place when the acidity level in the stomach is low (8). If low stomach acid is a prerequisite for infection, we might expect acid-suppressing drugs to increase the rate of infection and that is precisely what studies suggest (9).
So lets have a look at a potential progression here:
Low stomach acid > heartburn > acid suppressing drugs > H. pylori infection > further reduction of stomach acid > chronic heartburn and GERD.
H. Pylori increases your risk of developing bacterial overgrowth (SIBO) because that is what happens when the acid is too low, but it also impairs your ability to release bile from the gall bladder and digestive enzymes from the pancreas.
Roughly 90% of intestinal and 65% of gastric ulcers are caused by H pylori.
H.Pylori can be treated with antibiotics or, under the guidance of a functional health practitioner or naturopath, with anti-microbials. Such treatment should be accompanied with a course of probiotics. Also 500mg of Vitamin C a day helps keep H Pylori under control.
Connection between GERD and Stomach cancer
I have recently known two people who have had stomach cancer, and it isn’t pleasant. Atrophic gastritis is a major risk factor for stomach cancer. H. pylori is the leading cause of atrophic gastritis. Acid suppressing drugs worsen H. pylori infections and increase the rate of infection by H. pylori. Therefore it is not that huge a leap to say that acid suppressing drugs increase the risk of stomach cancer in those infected with H. pylori.
There is another way in which PPIs increase the risk of stomach cancer. Taking a standard daily dose of 20mg of Omeprazole typically results in a x3 – x4 increase in gastrin levels. Gastrin is a hormone, and above-normal secretion (hypergastrinemia) has been linked to adenocarcinoma – a form of stomach cancer. In people whose heartburn fails to respond to the standard dose of PPIs, long term-treatment with doses as high as 40-60mg is not uncommon. Such levels have produced gastrin levels as much as ten times higher than normal (10).
Connection between GERD and IBS, Crohn’s disease and Ulcerative Colitis
There is a very significant overlap between GERD and IBS. Roughly 2/3 of those who suffer with IBS also have GERD and 1/3 of GERD patients also have IBS. What this suggests is that IBS and GERD may very well share a common etiology and underlying mechanism.
It is well established that IBS is caused at least in part by SIBO (small intestinal bacterial overgrowth). It is also well known that acid-suppressing drugs contribute to bacterial overgrowth, as explained above. It makes sense then, that chronic use of these drugs can contribute to IBS in those that didn’t previously have it and worsen it in those that already were affected (11).
Adenosine is a molecule (a nucleoside, if you must) that occurs naturally in all cells of the body. It is essential for normal cell metabolism and growth. The point for you is that a high extracellular level is an important moderator of inflammation in the digestive tract, and hugely help in both Crohn’s disease and ulcerative colitis. Long term use of PPIs has been shown to decrease extracellular concentration of adenosine, resulting in inflammation in the digestive tract giving rise to potential serious inflammatory bowel disorders (12).
Connection between Low Stomach Acid and depression, anxiety and mood disorders
When you eat, stomach acid triggers the release of pepsin. Pepsin is the enzyme that breaks down protein into its component amino acids and peptides. If pepsin is deficient, the protein we eat wont be broken down into these components. Since many of these essential amino acids, such as phenylalanine and tryptophan, play a crucial role in mental and behavioural health, low stomach acid may predispose people towards developing depression, anxiety or mood disorders.
Connection between Low Stomach Acid and Leaky gut and Autoimmune disease
Low stomach acid and the consequential bacterial overgrowth, causes the intestine to become permeable, allowing undigested proteins to find their way between what should be tight junctions, into your bloodstream. This is often referred to as Leaky Gut. And it has been shown that leaky gut is substantially increased by atrophic gastritis (very low stomach acid) compared to control patients.
When undigested proteins end up in the bloodstream, they are considered as “foreign” by the immune system. The resulting immune response is similar to what happens when the body mobilises its defences (ie T cells, B cells and antibodies) to eradicate a viral or bacterial infection. A similar mechanism predisposes people with leaky gut to more serious autoimmune disorders, such as lupus, rheumatoid arthritis, type 1 diabetes, Graves disease, Crohn’s and ulcerative colitis.
The link between low stomach acid and rheumatoid arthritis is particularly well established. Swedish researchers found that 16 out of 45 (36%) rheumatoid arthritis patients had virtually no stomach acid. Those people who had RA for the longest, had the least acid (13).
Connection between Low Stomach Acid and Asthma
In the last decade more than 400 scientific articles looking at the connection between asthma and gastric acidity have been published. One of the most common features of asthma in addition to wheezing, is reflux. It is estimated that 80% of people with asthma also have GERD.
When acid gets into the windpipe that is a huge drop in the ability of the lungs to take in and breathe out air. Doctors who know of this association typically prescribe acid-suppressing drugs. While these do, of course, provide temporary relief, they don’t address the underlying cause that permitted the acid into the esophagus in the first place.